
Dr. Thomas Forbes (right) and Dr. Maral Ouzounian know life-saving medical devices make a difference but they come at a cost.
Tim Fraser
Life-saving devices
They restore hope and confidence, and they give people a second chance at life, but these devices aren’t cheap.
“Saving lives does not wait for coverage,” says Dr. Thomas Forbes, Surgeon-in-Chief of the Sprott Department of Surgery at University Health Network (UHN) and the James Wallace McCutcheon Chair in Surgery. This mantra is critical, especially when it comes to the many mechanical devices doctors implant on an almost regular basis.
Since the 1990s, the Centre has been outfitting patients with devices that drastically improve their quality of life, but if it weren’t for philanthropy, surgeons wouldn’t always have access to these costly pieces of equipment.
While the government eventually covers some of the cost, it’s because of donors that the Centre’s team can perform such complex operations.
“We don’t turn anybody down for surgery,” says Dr. Forbes. This sense of responsibility has become synonymous with the Centre’s global identity, and it’s also why it’s routinely chosen to provide cutting-edge equipment for patients who need it most.
$20,000
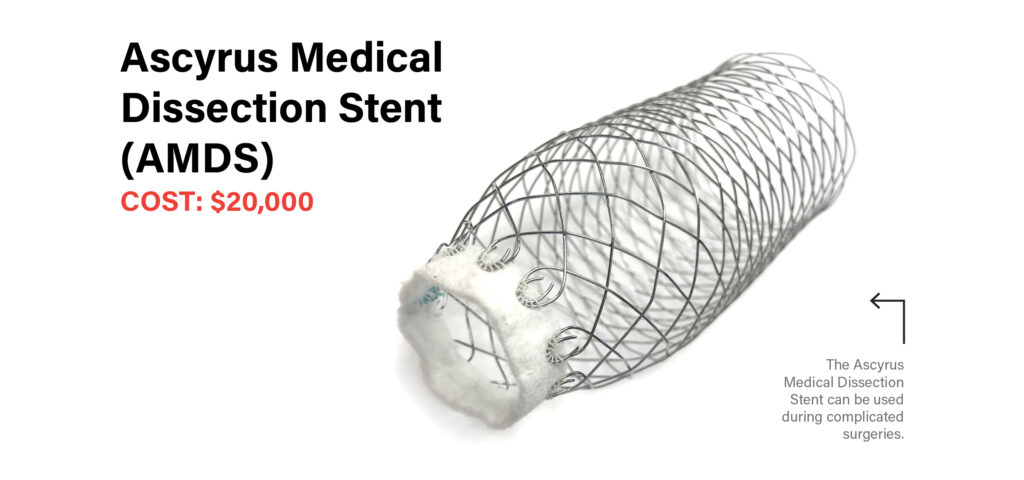
The cost of an Ascyrus Medical Dissection Stent (AMDS), a device approved by Health Canada for use at the Centre but is not yet funded by Ontario’s Ministry of Health. An AMDS gets implanted into the branched-off section of the aorta to help it heal and keep blood flowing through the proper channels.
Repairing ruptures
Ascyrus Medical Dissection Stent (AMDS)
Cost: $20,000
Last summer, Emily Keizer, 57, was about to set off into the bush to find chanterelle mushrooms with her husband. As she sat down to put on her boots, a searing pain tore through her chest and up through her shoulder blades. “It was horrible,” she says. The professional artist was rushed to the hospital in nearby Timmins, Ont.
A CT scan revealed that an aneurysm in the chest section of her aorta had ruptured and was limiting blood supply to the right side of her brain. Without immediate surgery she would have a severe stroke or die.
“We would not be able to use the needed devices without philanthropic support.”
Dr. Maral Ouzounian
Keizer was helicoptered to UHN’s Peter Munk Cardiac Centre, where a team led Dr. Maral Ouzounian, Head of Cardiac Surgery at the Peter Munk Cardiac Centre and Sprott Department of Surgery at UHN, who also holds the Munk Chair in Advanced Therapeutics and the Antonio & Helga De Gasperis Chair in Cardiovascular Surgery Clinical Trials and Outcomes Research, was ready even before she arrived. “When you tear the main blood vessel in your body, every branch that comes off it can be affected by the tear,” she says. Surgeons have always struggled to repair this part of the aorta, which supplies blood to the rest of the body. It wasn’t going to be an easy operation.
Fortunately, Dr. Ouzounian knew of a device that could make a difference: the Ascyrus Medical Dissection Stent, a dissection-specific hybrid prosthesis. The device, which is approved by Health Canada for use at the Centre but is not yet funded by Ontario’s Ministry of Health, resembles a tube of chicken wire made of fabric and metal that gets implanted into the branched-off section of the aorta to help it heal and keep blood flowing through the proper channels.
“We’re using the best equipment, the best techniques and the best people.”
Dr. Thomas Forbes
It’s so new that only a few sites in Canada have access to this specialized device. It was this access that enabled Dr. Ouzounian to successfully use this device to repair Keizer’s aorta after an intensive five-hour surgery. Had it not been for philanthropy, and the expertise of the Centre’s team, they wouldn’t have been able to use the stent that allowed Keizer to walk out of the surgery alive. After a week, she went home, where she picked up where she left off: hunting for mushrooms. “I can’t believe someone gave me the chance to be here,” she says.

$130,000
The cost of a Left Ventricular Assist Device (LVAD), often used as a permanent support for those deemed ineligible for transplant.
Keeping hearts beating
Left Ventricular Assist Device (LVAD)
Cost: $130,000
Mechanical hearts are a metal, battery operated pump that gets implanted directly into the heart and have traditionally been used as a temporary bridge to a transplant, keeping a patient alive as they wait to receive a new heart. Now, they’re often used as a permanent support for those who have been deemed ineligible for a transplant. People with LVADs find it life changing. “They have the energy to resume their daily activities and even do things that were once out of the question,” says Dr. Rao.
It was only in 2017, 16 years after the Peter Munk Cardiac Centre opened its mechanical heart program, that the government started funding the device for patients not eligible for transplant. It now funds 45 implants a year at the Centre. Before then, it was solely philanthropy that funded the first 200 devices.

Transcatheter aortic valve implant (TAVI)
Cost: $25,000
When the valve that connects the heart to the aorta becomes calcified, the opening narrows and prevents blood from flowing properly to the body.
“That’s a problem,” says Dr. Ouzounian. “Once the narrowing is severe and patients develop trouble breathing, 50 per cent die within two years.”
Fortunately, patients can undergo a TAVI procedure to replace the diseased valve without open-heart surgery. This device gets implanted via a catheter threaded through a blood vessel. The complex and life-saving procedure is only partially covered by the province.
Custom-made branched and fenstrated endografts
Cost: $35,000
An aneurysm is fatal if it ruptures. Those who have an aneurysm in the aorta in their chest must get it repaired so it doesn’t burst, but blood also needs to continue flowing through the aorta’s branches to the legs, kidneys, brain and more.
To repair these complex aneurysms in a minimally invasive way, doctors use an endovascular graft, which fits inside the aorta and looks like a “fancy toilet paper roll with branches,” says Dr. Forbes.
Since this graft has to fit perfectly, the manufacturer makes a custom device for each surgery. That requires careful imaging of the patient and extensive planning between the surgeon and the manufacturer.

